© 2025 Alltius Inc
Transportation Process Automation refers to the streamlining of patient transport and ambulance coordination workflows within TPA operations—especially critical in health insurance claim journeys. TPAs often serve as intermediaries between insurers, policyholders, hospitals, and ambulance vendors. But today, this coordination is largely manual, fragmented across emails, calls, and disconnected portals.
With automated processes, this becomes a real-time, system-driven process.
Automated Transport Requests
As soon as a hospitalization or discharge is initiated, TPAs can trigger automated processes like transport requests—based on location, policy coverage, hospital SLAs, and vendor availability.
Intelligent Vendor Matching
The system uses logic to match the best-fit ambulance or patient transport partner based on time, urgency, geography, and cost constraints—minimizing delays and reducing manual phone calls.
Live Status Tracking & Notifications
All stakeholders (hospitals, policyholders, vendors, TPAs) receive live updates on transport status, ETAs, and handoff confirmations via WhatsApp, email, or app-based alerts.
Auto-Documenting for Claims
Once the transport is completed, all documentation (trip sheets, driver details, timestamps) is captured and auto-attached to the policyholder's case file—simplifying downstream claims and audit requirements.
This is an example of a customer-value-added activity that improves downstream processing and reduces disputes.

As TPAs evolve from back-office engines to front-line experience managers, modern software isn’t just getting faster—it’s getting smarter. Intelligent automation is transforming how TPAs process documents, make decisions, detect fraud, and deliver service—all while unlocking measurable improvements in accuracy, responsiveness, and compliance. This includes leveraging technologies such as robotic process automation for structured, rule-based tasks.
At Alltius, we’ve seen firsthand how automation infused with machine learning, natural language processing, and large language models (LLMs) is changing the game.

TPAs deal with a flood of documents—claim forms, hospital invoices, handwritten notes, discharge summaries. Intelligent Document Processing (IDP) now combines OCR, NLP, and computer vision to not just extract—but understand—information. AI can pull diagnosis codes from messy medical reports or read policy numbers from scanned forms. Some platforms even link extracted data back to its source text—ensuring full auditability.
For TPAs, this isn’t just efficiency. It’s the value of customer experience quantified in insurance: faster onboarding, quicker claims, fewer data entry errors.
An example of a customer-value-added activity is eliminating rework from missing or misread data during claim intake.
Unlike traditional automation, which relies on static rule sets, AI support adapts to nuance. Historical data on claims allows models to predict potential fraud, settlement likelihood, or even claim severity before a human ever steps in. With the right context, LLMs can assess incoming requests and make smart recommendations—or auto-resolve simpler cases altogether.
For TPAs, that’s the shift from reactive to proactive. It ensures customers get faster outcomes, and human adjusters focus on where they’re most needed—raising the value of customer experience without bloating headcount.
The cost of fraud is rising. But so is AI’s ability to catch it. By analyzing large datasets—across billing patterns, medical histories, and claimant behavior—AI surfaces hidden anomalies like duplicate submissions or upcoded services. For TPAs, these systems act as always-on guardians, protecting clients from loss while ensuring fairness across the board through intelligent automation and robotic process automation frameworks.
AI-driven chat and email automation reduce the load on support desks and speed up customer response times. TPAs using these tools can now offer 24/7 coverage for status updates, eligibility queries, or documentation requests—all while personalizing the interaction.
Sentiment analysis adds another layer, flagging issues before they become complaints.
This shift—where routine interactions are automated and escalations are human-led—is core to delivering the value of customer experience in a transaction-based exchange.
It’s not about replacing people. It’s about focusing them on customer-value-added activities.
Regulatory complexity is only growing, but AI is stepping up. From validating documents against policy rules to logging every interaction for audit readiness, intelligent systems now monitor 100% of claim flows—not just a sample. This kind of end-to-end control is built using robotic process automation combined with dynamic logic layers.
Finally, AI isn’t just operational—it’s strategic. Predictive analytics can spot claim trends, cost drivers, or risk pockets across client portfolios. Instead of looking back at what happened, TPAs can guide insurers on what to expect—whether it’s adjusting reserves or shifting underwriting strategies.
That’s how TPAs move from service vendors to insight partners by translating the value of customer experience into actionable insights.
The rise of intelligent automation introduces a big question for insurers: do we bring these capabilities in-house or rely on forward-looking TPAs who already have them?
AI lowers the barrier for internal teams—but replicating the scale, specialization, and continuous improvement TPAs bring isn’t easy. Many insurers are finding that partnering with tech-enabled TPAs like those powered by Alltius gives them the best of both worlds: speed, control, and expertise.
Meanwhile, the TPA market is evolving fast. Legacy players that fail to adopt robotic process automation and AI risk getting edged out by nimble, AI-native competitors. Innovation is no longer optional—it’s the price of staying in the game.
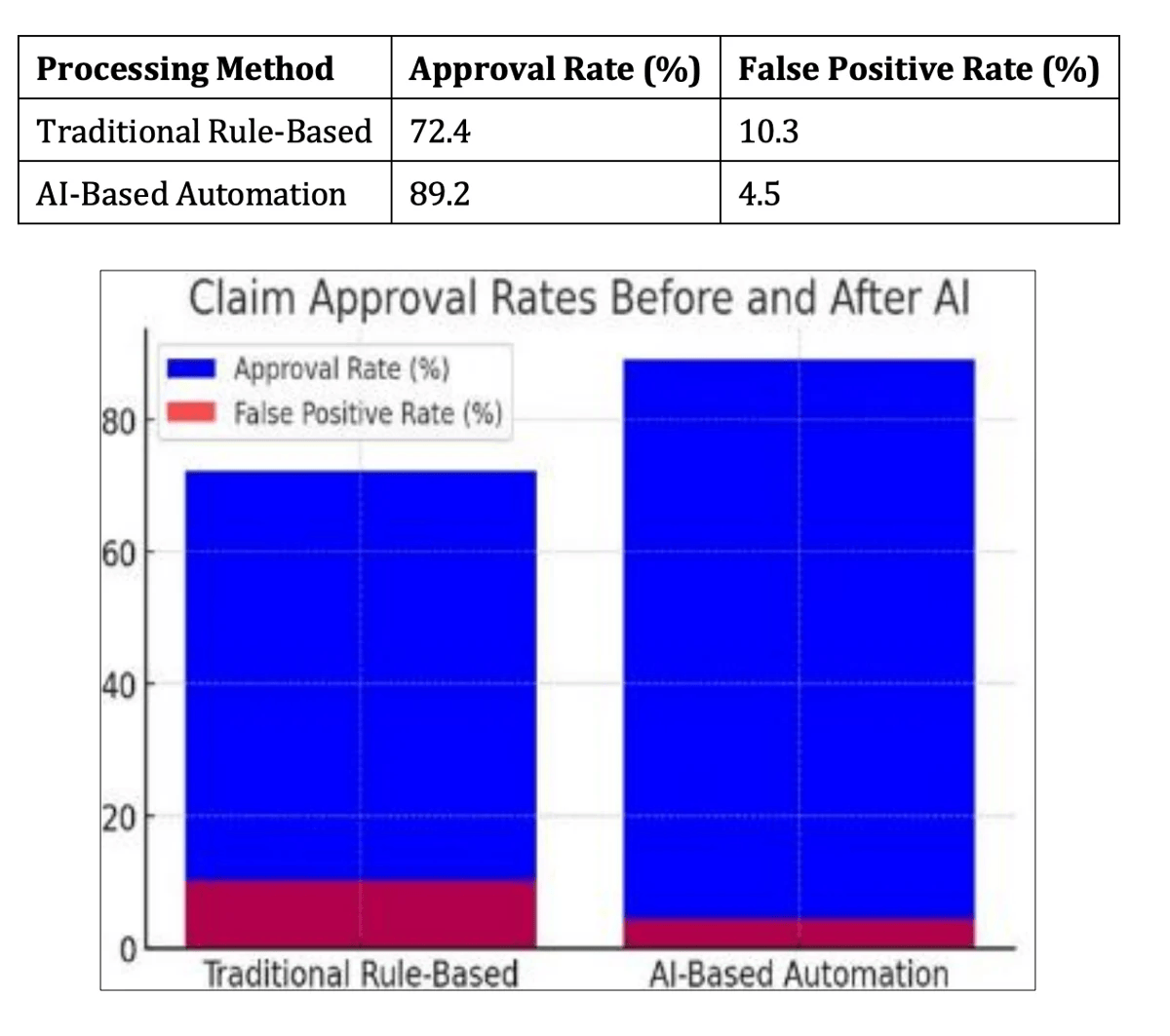
Forrester’s TEI studies paint a compelling financial picture:
These outcomes aren’t theoretical—they’re the value of customer experience quantified in health insurance through better routing, reduced delays, and real-time decisions.
Transportation Process Automation (TPA) is a crucial yet often overlooked element of the healthcare claims experience. Whether it’s arranging an ambulance at admission or coordinating patient discharge, these moments are time-sensitive and emotionally charged. Manual handling—phone calls, vendor delays, unclear documentation—only adds friction.

With Transportation Process Automation, this becomes a real-time, event-driven system:
When automated, this workflow improves speed, reduces disputes, and enhances trust—an example of a customer-value-added activity that elevates operational efficiency and service delivery.
In a transaction-based value exchange, transportation is one of the few high-emotion, high-impact touchpoints in the entire health insurance journey. It’s not just logistics—it’s a moment of truth. A well-coordinated ambulance can mean the difference between patient satisfaction and grievance escalation.
More importantly, automated processes like transport coordination directly improve:
Consider a health insurer processing 10,000 patient transport requests each month—ambulances for admissions, inter-facility transfers, or discharge support. Previously, a five-member coordination team earning ₹400k/year each managed this manually, spending ~8 minutes per request juggling calls, vendor follow-ups, and paperwork.
With Alltius:
The result? ~₹12 million in annual operational savings, fewer delays at critical moments, and dramatically improved patient and hospital satisfaction. That’s the value of customer experience quantified in health insurance—through automation that works when every minute counts.
To scale transportation automation effectively:
As McKinsey points out, even a 6%-7% improvement in time-sensitive CX processes can drive measurable gains in retention, trust, and brand equity—especially in healthcare settings where the cost of delay is high.
At Alltius, we don’t just plug in automation tools and hope for the best. We build purpose-driven, deeply integrated systems tailored to TPA workflows—ensuring impact from day one. Here’s how it works:
Alltius connects with your existing core systems—claims, enrollment, CRM, email—through secure APIs. We don’t force rip-and-replace. Instead, we overlay intelligent workflows on top of your tech stack to automate intake, triage, routing, and resolution across channels.
Our large language model (LLM)-based copilots are trained to understand insurance language—not just respond to it. They parse lengthy documents, classify inquiries, draft first responses, and summarize case history for agents.
We offer a visual builder for business teams and advanced developer tooling for complex logic—so TPAs can iterate fast.
Our automation engine continuously learns and improves. Every workflow is paired with tracking for volume, handle time, sentiment, and deflection.
Our structured onboarding model includes:
Because Alltius believes in measurable results, implementation milestones align with KPIs—contact deflection, handle time, satisfaction ratings, and renewal rates.
The evidence is unambiguous: effective CX automation isn’t optional—it’s business-critical. Digitized processes lift satisfaction, retention, and revenues while reducing cost and risk. For TPAs, this isn’t theory—it's a path to differentiation in a commoditized market.
Alltius specializes in translating those insights into action. They bridge the gap from static operations to dynamic CX—delivering ROI in months and building trust that stands the test of renewal cycles.
Want to dive deeper into a bespoke ROI model or a pilot blueprint? Happy to help map out your next step.
Or
Make life easier for your customers, agents & yourself with Alltius' all-in-one-agentic AI platform!
See how it works >>
Book a 30-minute demo & explore how our agentic AI can automate your workflows and boost profitability.

